- Your cart is empty
- Continue Shopping
Lung Cancer
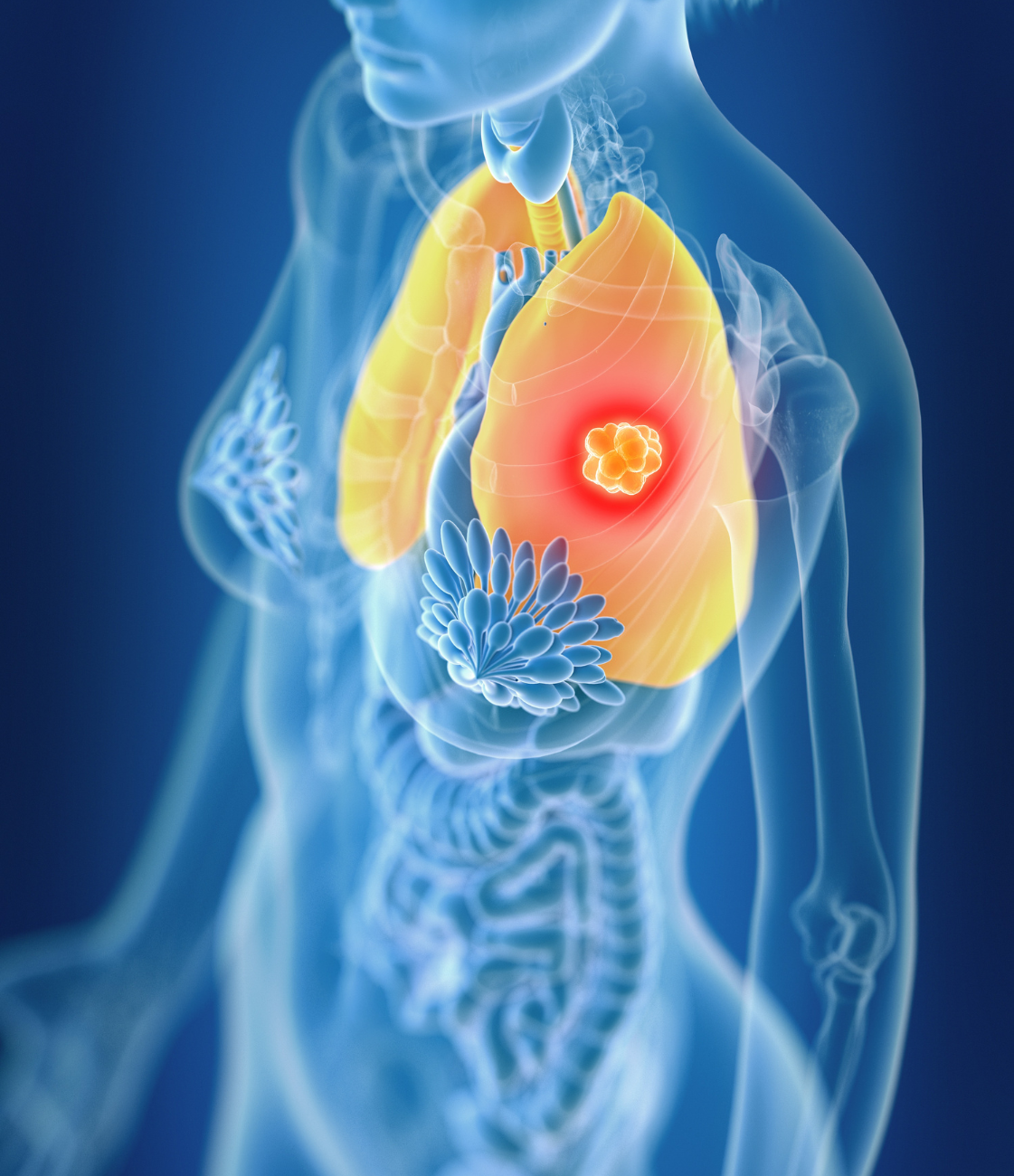
Lung Cancer
A Complete Guide by Medlama
Lung cancer is not just a medical condition — it is a life-altering journey that impacts millions across the globe, regardless of gender or age. It stands as one of the most common and deadliest forms of cancer worldwide, accounting for nearly 1 in 5 cancer-related deaths. The very organs that give us breath are affected, making this disease particularly daunting.
At Medlama, we understand the weight of a lung cancer diagnosis. The physical, emotional, and financial toll it takes on individuals and families can be overwhelming. That’s why we are not just focused on providing life-saving medicines — we are committed to walking with you through every phase of your journey.
We believe that knowledge is power. Raising awareness about early warning signs — such as persistent cough, chest pain, unexplained weight loss, and difficulty breathing — can lead to earlier diagnosis and better outcome.
What Increases the Chances of Lung Cancer?
Understanding the risk factors associated with lung cancer is crucial for prevention, early detection, and making proactive health decisions. While having a risk factor doesn’t mean you will definitely develop the disease, it does increase the likelihood. By identifying these risks early and making informed lifestyle changes, you can significantly lower your chances and improve your long-term health outcomes.
01. Smoking and Tobacco Use
Smoking is by far the leading cause of lung cancer, responsible for nearly 85% of all cases. Cigarettes, cigars, and pipes all contain harmful chemicals that damage lung cells. Over time, repeated exposure leads to mutations and uncontrolled cell growth. Even light or occasional smoking carries significant risk. The longer and more you smoke, the greater your chances. Quitting smoking at any stage greatly reduces this risk, though former smokers still remain at higher risk than non-smokers.
02. Secondhand Smoke Exposure
Even if you don’t smoke, frequent exposure to secondhand smoke can significantly increase your risk of lung cancer. Inhaling smoke from others contains the same cancer-causing agents as direct smoking and is particularly dangerous in enclosed spaces. Children, spouses, and co-workers of smokers are especially vulnerable.
03. Exposure to Radon Gas
Radon is a naturally occurring radioactive gas that can accumulate in homes, especially in poorly ventilated basements and ground floors. Long-term inhalation of radon gas is the second leading cause of lung cancer after smoking. It’s odorless and invisible, which makes testing your home environment essential—especially in regions with high radon levels.
04. Occupational Exposure to Carcinogens
Some professions involve exposure to cancer-causing substances, such as asbestos, arsenic, diesel exhaust, silica dust, and certain chemicals used in construction or manufacturing. Individuals working in mining, construction, shipbuilding, or heavy industry are often at higher risk, especially if protective measures are not strictly followed.
05. Air Pollution
Long-term exposure to outdoor air pollution, especially in densely populated or industrial areas, contributes to lung cancer risk. Tiny particles from vehicle exhaust, factories, and burning fossil fuels can reach deep into the lungs and damage tissue over time. According to the World Health Organization, air pollution is classified as a Group 1 carcinogen — the same category as tobacco smoke.
06. Personal or Family History of Lung Disease or Cancer
If you’ve had lung cancer before, there’s an increased risk of developing it again. A family history of lung cancer may also increase your susceptibility, even if you’ve never smoked. This may be due to shared genetic mutations or environmental exposures. Additionally, chronic lung diseases such as chronic obstructive pulmonary disease (COPD) or pulmonary fibrosis can further elevate your risk.




Early Awareness
What is Lung Cancer?
Lung cancer begins when abnormal cells in the lungs start to grow uncontrollably. These cells can form a tumor, which interferes with the normal function of the lungs, making it difficult to breathe and absorb oxygen. As the disease progresses, these cancerous cells may invade nearby tissues or spread (metastasize) to other parts of the body, such as the brain, bones, liver, or adrenal glands.
There are two main types of lung cancer, classified based on how the cells appear under a microscope. The most common is Non-Small Cell Lung Cancer (NSCLC), which accounts for approximately 85% of all cases. It generally grows more slowly than Small Cell Lung Cancer and includes subtypes such as Adenocarcinoma (commonly seen in non-smokers and women), Squamous Cell Carcinoma, and Large Cell Carcinoma. The second type is Small Cell Lung Cancer (SCLC), which makes up about 10–15% of lung cancer cases. It is more aggressive, tends to grow and spread rapidly, and is strongly associated with smoking. Due to its fast progression, it is often diagnosed at an advanced stage and requires intensive treatment.

Hidden Warnings
Signs and Symptoms of Lung Cancer
Yes, shortness of breath, wheezing, and chest pain (especially when coughing or laughing) can be signs that the cancer is affecting lung function or surrounding tissues. These symptoms often become more noticeable as the disease progresses.
Look for unexplained weight loss, fatigue, and loss of appetite. Swelling in the face or neck, frequent respiratory infections like bronchitis or pneumonia, and pain in the shoulder or back can also be warning signs of lung cancer.
Yes. Coughing up blood (hemoptysis), even in small amounts, is a serious symptom that requires immediate medical attention. Additionally, changes in the voice, such as persistent hoarseness, can occur if the tumor affects the nerves that control the vocal cords.
Not necessarily. Many of these symptoms can also be caused by less serious conditions like infections or chronic bronchitis. However, if symptoms persist, worsen, or appear suddenly, it's important to consult a healthcare provider for proper diagnosis and timely intervention. Early detection saves lives.
Lung Cancer Medicines Available at Medlama
At Medlama, we understand how vital timely and reliable access to lung cancer treatments is for patients and their families. That’s why we offer a carefully selected range of FDA-approved, WHO-GMP certified, and internationally recommended medications — sourced exclusively from trusted manufacturers. Whether the patient is dealing with non-small cell lung cancer (NSCLC) or small cell lung cancer (SCLC), our portfolio includes targeted therapies, chemotherapy drugs, and immunotherapy options, tailored to support every stage of treatment.
Gefitinib (Iressa)
Gefitinib is a targeted therapy used primarily in EGFR-mutated non-small cell lung cancer (NSCLC). It works by blocking signals that cancer cells need to grow. Gefitinib is typically prescribed as a first-line oral treatment in patients whose tumors have tested positive for EGFR mutations, often offering fewer side effects than traditional chemotherapy.
Erlotinib (Tarceva)
Erlotinib is another EGFR inhibitor used in advanced or metastatic NSCLC. It prevents the growth of cancer cells by targeting specific enzymes. Erlotinib is especially effective in non-smokers or light smokers with specific genetic markers and is often used when chemotherapy is not well-tolerated.
Osimertinib (Tagrisso)
Osimertinib is a third-generation EGFR inhibitor used for advanced NSCLC patients with T790M mutation or as a first-line therapy in EGFR-mutant lung cancer. It crosses the blood-brain barrier, making it an effective option for patients with brain metastases. It is known for its high precision and low toxicity.
Crizotinib (Xalkori)
Crizotinib is a targeted oral therapy used in NSCLC patients with ALK or ROS1 gene rearrangements. It works by blocking abnormal proteins that promote cancer growth. Crizotinib has transformed outcomes in certain genetic subtypes of lung cancer and is widely recommended in personalized cancer care.
Atezolizumab (Tecentriq)
Atezolizumab is an immunotherapy drug (a PD-L1 inhibitor) used for advanced NSCLC and sometimes SCLC. It helps the immune system recognize and destroy cancer cells. It is often used alone or in combination with chemotherapy and has shown promising survival benefits in both first-line and later-line settings.
Carboplatin & Paclitaxel
This chemotherapy combination is commonly used in both NSCLC and SCLC. Carboplatin interferes with the cancer cell’s DNA, while Paclitaxel prevents cell division. Together, they form the backbone of many first-line chemotherapy regimens, especially in advanced or unresectable lung cancer cases.
At Medlama, we are committed to supporting every lung cancer patient with expert guidance, authentic medicines, and timely delivery. Our knowledgeable team ensures that each prescription is accompanied by clear usage instructions, cold-chain storage (if required), and follow-up support for a smoother treatment experience.
Welcome to Medlama — a holistic healing initiative under Narang Biotec — designed to support your emotional and mental wellbeing alongside medical treatment.
At Medlama, we believe that healing is not just physical — it’s also emotional, spiritual, and mental. Our aim is simple: to create a safe, empowering space where we can come together to beat cancer with strength, positivity, and support — beyond medicine.
Useful Links
Address
- 3966, 2nd Floor, Roshanara Rd, Arya Pura, Sabzi Mandi Old, New Delhi, Delhi 110007
- +91-9205022032
- contact@medlama.com
