- Your cart is empty
- Continue Shopping
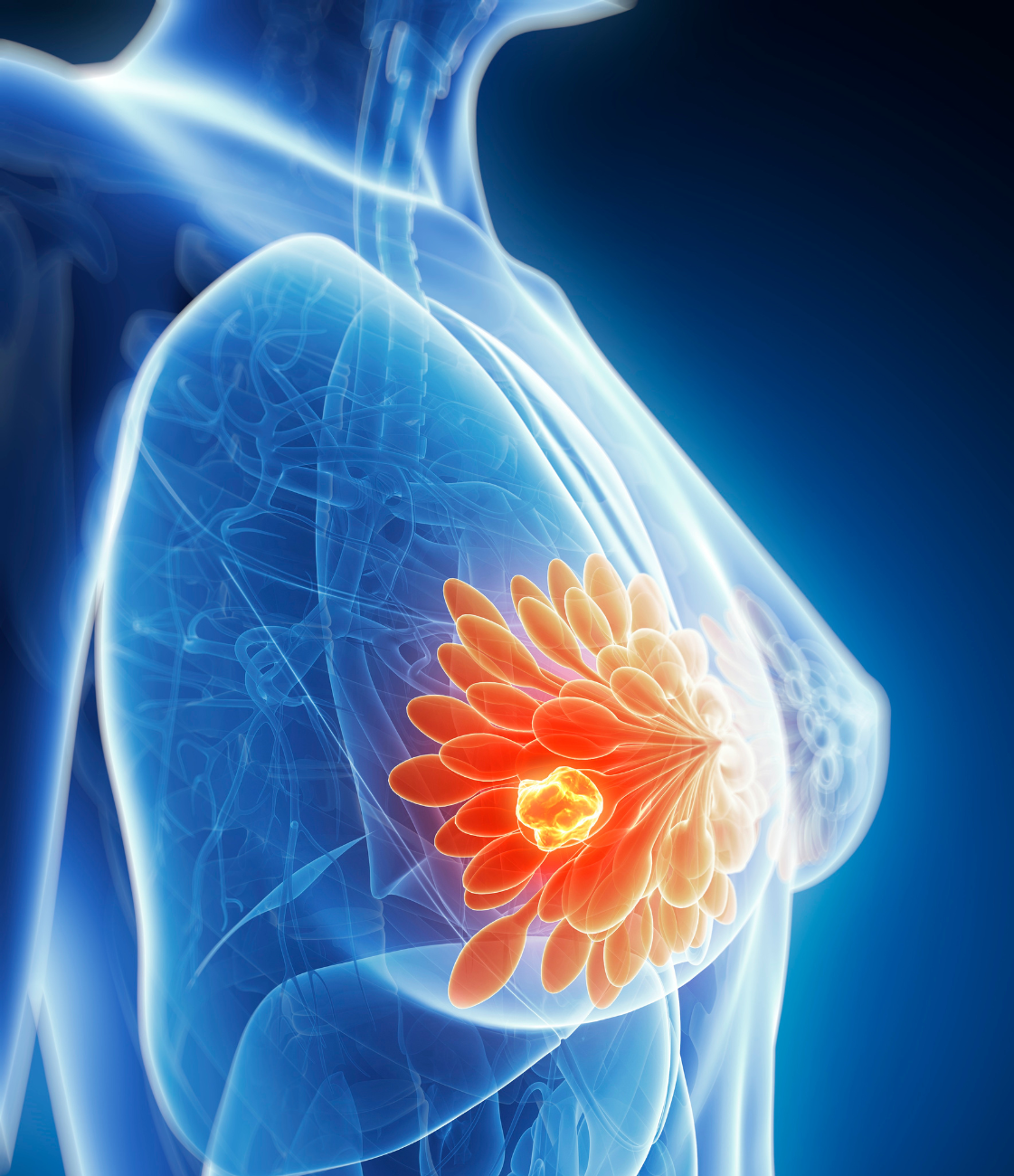
Breast Cancer

Breast Cancer
A Complete Guide by Medlama
Breast cancer is not just a disease; it’s a challenge that touches the lives of millions globally. It is the most common cancer among women worldwide, accounting for nearly 25% of all cancer cases in females. While the diagnosis can be overwhelming, early detection and effective treatment significantly improve outcomes.
At Medlama, we are committed to supporting you through every step — from awareness to access to genuine medicines and emotional support.
At Medlama, we believe that awareness is the first step toward prevention and empowerment. Our goal is not just to provide life-saving medicines but to create a support system where every patient feels informed, cared for, and never alone. Through partnerships with leading oncologists, diagnostic centers, and support groups, we ensure that every individual receives personalized guidance, access to affordable treatment, and the emotional strength needed to fight breast cancer with dignity and hope.
What Increases the Chances of Breast Cancer?
Understanding the risk factors associated with breast cancer is essential for prevention, early detection, and making informed lifestyle choices. While having one or more risk factors does not guarantee that you will develop the disease, it does increase the likelihood. Being aware of these risks empowers you to take proactive steps for your health through regular screenings, healthier habits, and timely consultations with healthcare providers.
01. Age
Age is one of the strongest risk factors for breast cancer. The chances of developing the disease rise significantly as women get older. Women over 40 are considered at higher risk, and the likelihood increases even more after the age of 50. This is primarily due to the cumulative exposure of breast tissue to genetic mutations and hormonal changes over time. As a result, regular mammogram screenings are highly recommended starting at age 40 to ensure early detection.
02. Genetics and Inherited Mutations
Some women inherit mutations in specific genes that increase their risk of breast cancer. The most common ones are BRCA1 and BRCA2. Women who carry these mutations may face up to an 80% lifetime risk of developing breast cancer. Genetic testing and counseling are especially important if you have a strong family history of breast or ovarian cancer. Identifying these mutations early allows for preventive steps such as increased monitoring or even preventive surgery in some cases.
03. Family History
Having a first-degree relative (like a mother, sister, or daughter) with breast or ovarian cancer increases your own risk. The risk is greater if multiple relatives are affected or if they were diagnosed at a young age. However, it’s important to note that around 85% of women diagnosed with breast cancer have no family history, which highlights the importance of routine screening and awareness for all women, regardless of family background.
04. Hormonal Factors
Hormonal fluctuations throughout a woman’s life can influence breast cancer risk. For instance, an early onset of menstruation (before age 12) or late menopause (after age 55) results in longer lifetime exposure to estrogen and progesterone, which can promote the development of certain breast cancers. Additionally, the use of hormone replacement therapy (HRT) during or after menopause has been linked to increased risk, particularly when used over a long period.
05. Lifestyle & Environmental Factors
Modern lifestyle habits play a significant role in increasing the risk of breast cancer. Factors such as poor diet, lack of physical activity, smoking, and alcohol consumption can negatively impact hormone levels, cause chronic inflammation, and damage healthy cells. Obesity, particularly after menopause, leads to higher estrogen levels stored in fat tissue and promotes inflammation, both of which are known to support cancer cell growth. Smoking introduces carcinogenic compounds that harm breast tissue over time and are associated with multiple cancers. Alcohol, even in small quantities, elevates estrogen levels and can cause DNA damage, further raising the risk. Additionally, a sedentary lifestyle contributes to hormonal imbalances and weight gain, whereas regular physical activity — like 30 minutes of brisk walking daily — can significantly reduce the likelihood of developing breast cancer.
06. Reproductive History
Certain reproductive choices and conditions affect hormone levels and therefore influence breast cancer risk. Women who have their first child after age 30, do not breastfeed, or have never had children tend to have a slightly higher risk. These factors are thought to affect the body’s natural hormonal exposure over time.



Early Awareness
What is Breast Cancer?
Breast cancer starts when abnormal cells in the breast begin to grow out of control. These cells usually form a tumor that can be seen on an X-ray or felt as a lump. The tumor is malignant (cancerous) if the cells can grow into (invade) surrounding tissues or spread (metastasize) to distant areas of the body
There are several types of breast cancer, the most common being:
Invasive Ductal Carcinoma (IDC)
Invasive Lobular Carcinoma (ILC)
Ductal Carcinoma In Situ (DCIS)
Triple Negative Breast Cancer (TNBC)
HER2-Positive Breast Cancer
Each type requires a different treatment approach, which is why correct diagnosis is critical.

Hidden Warnings
Signs and Symptoms of Breast Cancer
Yes. Swelling or thickening of a part of the breast, even without a distinct lump, can be an early warning sign and should not be ignored.
Look for irritation, dimpling, or puckering of the breast skin — this may resemble the texture of an orange peel and could indicate an underlying tumor.
Yes. Watch for redness, dryness, scaling, or flaky skin in the nipple area. These could be signs of breast cancer or a rare condition like Paget’s disease.
Not necessarily. These symptoms may also be caused by infections, cysts, or hormonal changes. However, it's critical to get them checked by a healthcare professional to rule out cancer.
Breast Cancer Medicines Available at Medlama
At Medlama, we understand how crucial it is for patients to receive timely access to reliable and effective breast cancer treatments. That’s why we offer a carefully curated range of FDA-approved, WHO-GMP certified, and globally recommended medications — sourced only from trusted, verified manufacturers. Whether it’s early-stage or advanced breast cancer, our selection includes targeted therapies, hormonal treatments, and oral chemotherapy options, tailored to match each patient’s specific diagnosis and treatment plan.
Tamoxifen
Tamoxifen is one of the most commonly prescribed hormonal therapies for estrogen receptor-positive (ER+) breast cancer. It works by blocking estrogen receptors in breast cells, effectively preventing the hormone from stimulating cancer growth. Tamoxifen is often used in both pre- and postmenopausal women, and can be prescribed for several years after initial treatment to reduce the risk of recurrence.
Letrozole (Femara)
Letrozole is an aromatase inhibitor mainly used in postmenopausal women. It functions by lowering estrogen levels in the body, which slows or stops the growth of hormone-sensitive tumors. Letrozole is frequently prescribed as an adjuvant therapy following surgery or in cases where Tamoxifen is not effective.
Anastrozole (Arimidex)
Similar to Letrozole, Anastrozole is also an aromatase inhibitor used in ER+ breast cancer. It reduces estrogen production in the body and is commonly used as part of adjuvant therapy to prevent cancer recurrence in postmenopausal women. It is well-tolerated and often chosen for long-term maintenance therapy.
Trastuzumab (Herceptin)
Trastuzumab is a targeted monoclonal antibody therapy specifically designed for HER2-positive breast cancer. It works by binding to the HER2 protein on the surface of cancer cells, inhibiting their growth and signaling the immune system to destroy them. Herceptin is often used in combination with chemotherapy or other HER2-targeted drugs.
Capecitabine (Xeloda)
Capecitabine is an oral chemotherapy medication commonly used in patients whose cancer has metastasized (spread) or returned after other treatments. It is converted into its active form inside cancer cells, where it disrupts DNA synthesis and inhibits tumor growth. Its convenience as a pill makes it a preferred option in outpatient settings.
Fulvestrant (Faslodex)
Fulvestrant is an estrogen receptor antagonist used primarily for advanced hormone receptor-positive breast cancer in postmenopausal women. It works by degrading estrogen receptors, unlike Tamoxifen which blocks them. Fulvestrant is typically administered when other hormonal therapies have stopped being effective.
At Medlama, our team is committed to guiding you through each step of your treatment journey with the right medicine, clear instructions, and proper follow-up. All medicines are handled under controlled conditions to ensure potency, safety, and timely delivery.
Welcome to Medlama — a holistic healing initiative under Narang Biotec — designed to support your emotional and mental wellbeing alongside medical treatment.
At Medlama, we believe that healing is not just physical — it’s also emotional, spiritual, and mental. Our aim is simple: to create a safe, empowering space where we can come together to beat cancer with strength, positivity, and support — beyond medicine.
Useful Links
Address
- 3966, 2nd Floor, Roshanara Rd, Arya Pura, Sabzi Mandi Old, New Delhi, Delhi 110007
- +91-9205022032
- contact@medlama.com
