- Your cart is empty
- Continue Shopping
Cervical Cancer
Cervical Cancer
A Complete Guide by Medlama
Cervical cancer is one of the most preventable yet life-threatening cancers affecting women, especially in low- and middle-income countries. It develops slowly and is primarily caused by persistent infection with high-risk types of the human papillomavirus (HPV). Despite being preventable through regular screening and vaccination, thousands of women are still diagnosed at later stages due to lack of awareness and access to care.
At Medlama, we are dedicated to changing this reality — by spreading awareness, facilitating timely diagnosis, and ensuring access to authentic, WHO-GMP certified cervical cancer medicines.
We believe that informed choices save lives. That’s why our mission goes beyond just delivering treatment. We aim to build a circle of care — connecting patients to leading gynecologic oncologists, diagnostic labs, and emotional support networks. Every woman deserves a chance to detect cervical cancer early, access affordable care, and receive the strength to recover with dignity and resilience.
What Increases the Chances of Cervical Cancer?
Understanding the risk factors associated with cervical cancer is crucial for prevention, early detection, and informed healthcare decisions. Although having one or more of these factors does not mean you will develop cervical cancer, it does increase the likelihood. By staying informed and proactive — through regular screenings like Pap smears and HPV tests — you can significantly reduce your risk and improve long-term outcomes.
01. Human Papillomavirus (HPV) Infection
The most significant risk factor for cervical cancer is infection with high-risk strains of the human papillomavirus (HPV), particularly types 16 and 18. HPV is a common sexually transmitted infection, and most people clear it naturally. However, persistent infection with high-risk HPV types can cause changes in the cervix that may lead to cancer over time. HPV vaccination and regular screening are key preventive measures.
02. Early Sexual Activity and Multiple Partners
Becoming sexually active at a young age or having multiple sexual partners increases the risk of HPV exposure, thereby raising the chances of cervical cell changes. This is because HPV is transmitted through intimate skin-to-skin contact, and increased exposure elevates the likelihood of infection.
03. Weakened Immune System
A compromised immune system — due to conditions like HIV/AIDS or use of immunosuppressive medications (e.g., after organ transplant) — reduces the body’s ability to fight off HPV infections. This makes it harder to clear the virus and increases the risk of cervical precancer and cancer.
04. Smoking
Tobacco use introduces harmful chemicals into the body that can damage the DNA of cervical cells. Smoking also weakens the immune system’s ability to clear HPV infections. Women who smoke are about twice as likely to develop cervical cancer compared to non-smokers.
05. Long-Term Use of Oral Contraceptives
Research suggests that using birth control pills for five or more years may slightly increase the risk of cervical cancer. The hormonal changes caused by prolonged contraceptive use may make cervical cells more vulnerable to HPV infection. However, the risk typically returns to normal after stopping the pills for a few years.
06. Multiple Full-Term Pregnancies
Women who have had three or more full-term pregnancies may have an increased risk of cervical cancer. Hormonal changes and physical changes in the cervix during pregnancy, along with potential increased exposure to HPV, may contribute to this risk.


Early Awareness
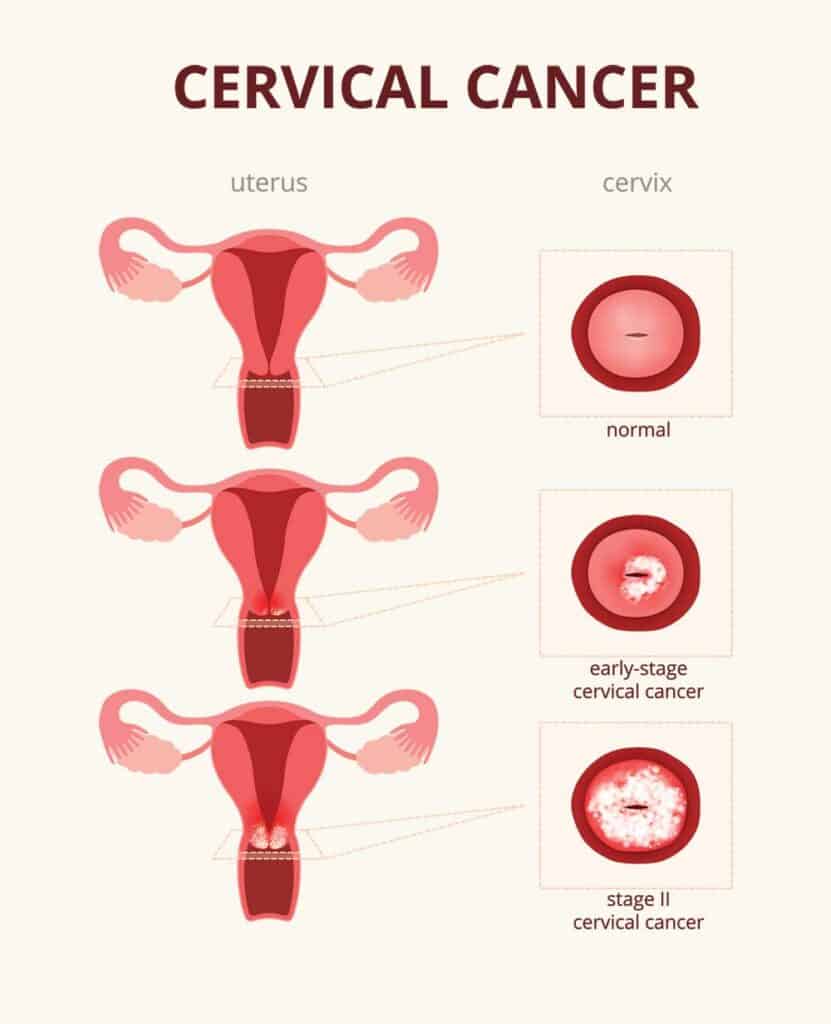
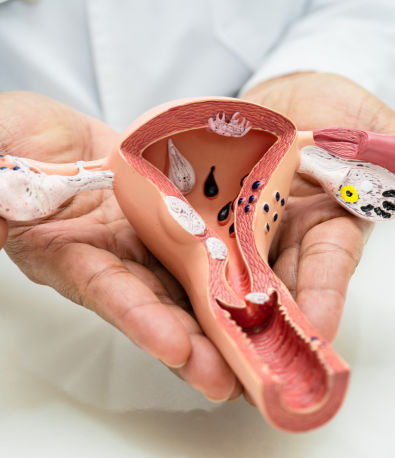
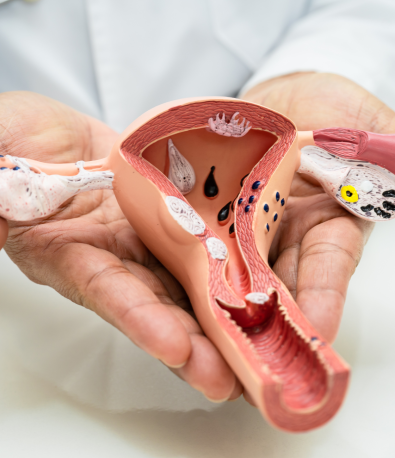
What is Cervical Cancer?
Cervical cancer starts in the cells of the cervix, the lower part of the uterus that connects to the vagina. It’s most often caused by persistent infection with high-risk human papillomavirus (HPV). Over time, these abnormal cell changes can lead to cancer if not detected early.
The disease typically develops slowly, making it highly preventable through routine Pap smears and HPV testing.
Squamous Cell Carcinoma
The most common type, arising from the outer layer of the cervix (about 80–90% of cases).Adenocarcinoma
Develops in mucus-producing glandular cells inside the cervical canal.Adenosquamous Carcinoma
A rarer, more aggressive type containing both squamous and glandular cells.

Hidden Warnings
Signs and Symptoms of Cervical Cancer
Yes. Women with cervical cancer may notice watery, pink, or foul-smelling vaginal discharge. This can occur due to tumor irritation or infection and should not be ignored.
Persistent pelvic pain, lower back pain, or pain during sex (dyspareunia) can be signs of advanced cervical cancer. These symptoms often indicate the cancer has started affecting surrounding tissues.
Yes. In more advanced stages, cervical cancer can cause difficulty urinating, blood in urine, or even constipation if it presses against nearby organs. These signs should be checked immediately.
Not necessarily. These symptoms can also be caused by infections, fibroids, or other conditions. However, early evaluation is key — especially if symptoms persist. Regular Pap smears and HPV tests help detect issues before they become serious.
Cervical Cancer Medicines Available at Medlama
At Medlama, we are dedicated to ensuring patients have timely and reliable access to the most effective cervical cancer treatments. We offer a carefully selected range of FDA-approved, WHO-GMP certified, and globally trusted medications — sourced only from verified manufacturers. Whether it’s early-stage cervical cancer or advanced/metastatic disease, our medicines are chosen to align with the patient’s treatment plan, condition, and stage of diagnosis.
Our offerings include chemotherapy agents, targeted therapies, and immunotherapy options, tailored for better outcomes and improved quality of life.
Cisplatin
Cisplatin is a platinum-based chemotherapy drug commonly used as a first-line treatment for cervical cancer. It works by damaging the DNA of cancer cells, preventing them from dividing and growing. Often used alone or in combination with radiation therapy (chemoradiation), Cisplatin remains a cornerstone in cervical cancer treatment.
Carboplatin
An alternative to Cisplatin with a similar mechanism but a different side effect profile, Carboplatin is often used in patients who may not tolerate Cisplatin well. It is also used in combination with other chemotherapy drugs for recurrent or advanced cervical cancer.
Paclitaxel (Taxol)
Paclitaxel is a chemotherapy drug that inhibits cancer cell division by stabilizing microtubules. It is frequently combined with platinum-based drugs like Cisplatin or Carboplatin in the treatment of advanced or recurrent cervical cancer.
Bevacizumab (Avastin)
Bevacizumab is a targeted monoclonal antibody that blocks the growth of blood vessels that feed tumors (anti-angiogenic therapy). It is used in combination with chemotherapy for advanced cervical cancer and has been shown to improve survival in certain patients.
Topotecan
Topotecan is a topoisomerase I inhibitor used in second-line treatment for recurrent cervical cancer. It works by interfering with the enzymes needed for cancer cell replication and is often used when the disease progresses after initial chemotherapy.
Fulvestrant (Faslodex)
Fulvestrant is an estrogen receptor antagonist used primarily for advanced hormone receptor-positive breast cancer in postmenopausal women. It works by degrading estrogen receptors, unlike Tamoxifen which blocks them. Fulvestrant is typically administered when other hormonal therapies have stopped being effective.
At Medlama, we go beyond simply delivering medicines — we ensure you receive the right guidance, proper instructions, and personalized care throughout your treatment journey. Every medicine is stored and shipped under strict conditions to maintain safety, efficacy, and timely access when it matters most.
Welcome to Medlama — a holistic healing initiative under Narang Biotec — designed to support your emotional and mental wellbeing alongside medical treatment.
At Medlama, we believe that healing is not just physical — it’s also emotional, spiritual, and mental. Our aim is simple: to create a safe, empowering space where we can come together to beat cancer with strength, positivity, and support — beyond medicine.
Useful Links
Address
- 3966, 2nd Floor, Roshanara Rd, Arya Pura, Sabzi Mandi Old, New Delhi, Delhi 110007
- +91-9205022032
- contact@medlama.com
